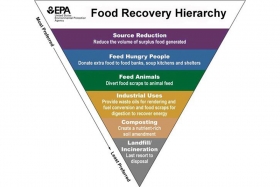
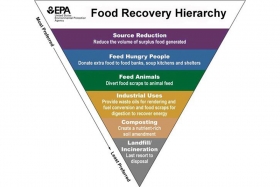
Reducing Food Waste in Foodservice
October 16, 2018 by Doreen Garelick, Dietetic Intern
Our intern Doreen attended a food waste summit for restaurants and compiled these tips to help food service operators redirect…
May 29, 2018

Earlier this spring, first reports came out of romaine lettuce contamination with e.coli O157. While the CDC now reports it is highly unlikely that there is any contaminated romaine lettuce left on shelves, until recently recommendations were to avoid romaine lettuce altogether unless confirmed it was not grown in the Yuma, AZ region which was identified as the source of contamination. At SPE, we are the first to promote increased intake of fruits and vegetables and we certainly don’t want this latest outbreak to discourage people from eating their leafy greens but it did make us want to take a closer look at the incidence of pathogen contamination in produce versus meat.
Each year, 128,000 Americans are hospitalized and 3,000 die from foodborne illnesses. Eight known pathogens are estimated to account for the majority of domestically acquired foodborne illnesses, hospitalizations, and deaths. The top 5 pathogens that result in hospitalizations are: salmonella, norovirus, campylobacter spp., toxoplasma gondii, and e.coli O157.
Usually associated with raw or uncooked seafood, meat, poultry, and eggs, most of the recent food-borne illness outbreaks have been linked to a variety of foods other than animal products - in fact, several have been linked to raw produce. For example, while salmonella has been historically linked to raw eggs, only 3 of the past 63 outbreaks of salmonella have been linked to shell eggs. The Center for Science in the Public Interest (CSPI) came out with a report in 2010 that revealed similar data, making it clear that outbreaks linked to produce are much more common than other food groups.
And although historically called “the Hamburger disease”, of the past 30 reported outbreaks of e.coli O157 since 2006, only 8 were linked to beef. E.coli bacteria live in the intestinal tracts of humans and animals and e.coli O157 is a particular strain that damages the lining of the small intestine and can cause severe abdominal cramps, vomiting and bloody diarrhea. Exposure to e.coli O157 is from contaminated food or water. The reason it is commonly associated with ground beef is because the e.coli bacteria from cattle’s intestines can get onto the meat during slaughtering and processing and because packaged ground beef typically includes meat from multiple different cows, there is a higher risk of contamination. If contracted, healthy adults can recover from the infection within a week, but young children and older adults can develop kidney failure (hemolytic uremic syndrome) which can be life threatening.
The Most Recent Outbreak
But as is evidenced by recent outbreaks, the incidence of e.coli O157 is not just in ground beef but is also found in produce. In fact, leafy greens have been attributed to the cause of roughly a fifth of all foodborne illnesses.
What has caused the most attention in the news is the recent multistate outbreak of e.coli O157 found in romaine lettuce. As of May 16, 2018, there were 172 cases reported across 32 states. Illnesses started on dates ranging from mid March to mid April among ages 1 to 88 years. According to the CDC, of 157 people with information available, 75 (48%) have been hospitalized, including 20 people who developed hemolytic uremic syndrome, a type of kidney failure and one death was reported from California. It is the largest American e. coli outbreak since 2006 when tainted spinach sickened almost 200 people across 26 states.
Why Produce?
One indirect reason we are seeing more reports of foodborne illness linked to produce may be because Americans are eating more fresh produce than in the past so there is more exposure. However there are other factors that increase the risk of contamination of raw produce. First, produce can become contaminated with e.coli O157 when it comes into contact with animal or human waste. For example, fields where fresh produce is grown can be contaminated from runoff from cattle farms or contaminated irrigation water. And there can be cross-contamination during processing, particularly when lettuces from multiple farms are co-mingled for pre-packaged salad mixes or when produce is grown on farms where animals are also raised. Lastly, certain foods such as sprouts are grown in conditions that promote bacterial growth and are typically consumed raw so any pathogenic bacteria would remain.
Thus far in the recent romaine lettuce case, investigators have identified the general area of contamination as the Yuma, AZ, growing region but not the specific source of contamination along the chain of growing, harvesting, processing and distributing. To put this into perspective as to how challenging this is to trace, Yuma County is ranked third in the nation for vegetable production and 90% of all leafy vegetables grown in the US from November through March are grown in and around Yuma. Furthermore, the region includes nine facilities that produce bagged lettuce and salad mixes.
Romaine lettuce also comes in many forms: conventional, organic, whole head, unwashed or pre-washed, cored, chopped, or mixed in bags with other lettuces. The more processed the lettuce is, the more opportunities there are for contamination.
Because investigators were unable to pinpoint a source of contamination beyond the general region, initial recommendations were to avoid eating romaine lettuce unless confirmed it was not from the Yuma region. However now, according to the FDA, the last shipments of romaine from the Yuma were on April 16 and because romaine lettuce has a 3 week shelf-life, it should no longer be on any grocery store shelves or served in restaurants so you can finally resume eating romaine again.
How To Reduce Your Risk?
E.coli O157 is destroyed with heat so if you are consuming ground beef, make sure you cook it to an internal temperature of 160F.
However produce is trickier as it is difficult to remove pathogenic bacteria from leafy greens since there are many crevices for bacteria to adhere to on the surface of the leaves or on the interior. Washing can remove some but not all bacteria and has not been proven to be an effective way to remove harmful e.coli.
Cooking leafy greens is the only way to truly destroy any present e.coli or salmonella. But if you aren’t ready to cook your salad, the most important thing you can do is to practice good human hygiene and safe food handling at home to minimize any risk of cross-contamination. Here are some great tips from the FDA on safe food handling.
October 16, 2018 by Doreen Garelick, Dietetic Intern
Our intern Doreen attended a food waste summit for restaurants and compiled these tips to help food service operators redirect food waste from landfills.
Nutrition 101

Nutrition 101
September 26, 2018 by Doreen Garelick, Dietetic Intern
Ever notice headlines about rapid weightloss? Dietetic Intern Doreen Garelick looks deeper into a recent eye-catching headline to see if there's any truth behind it.
Connect
 Follow us on Twitter
Follow us on Twitter Friend us on Facebook
Friend us on Facebook Follow us on Pinterest
Follow us on Pinterest Follow us on Instagram
Follow us on Instagram Read our Blog
Read our Blog Watch videos on YouTube
Watch videos on YouTube Watch videos on Vimeo
Watch videos on Vimeo Connect with us on Linkedin
Connect with us on Linkedin Find us on Foursquare
Find us on Foursquare
Tweets by @SPEcertifiedBlog Search
Categories
SPE Certified Newsletter
Sign up for news on the latest SPE-certified venues, events and SPE updates.
We will never share your personal information with a third party.